
A person can be very literate but still struggle with health literacy.
Health literacy is not the same as general literacy—that is, the ability to read and write. Nor is it simply being able to read or listen to basic information about their health.
To be truly health literate, a person needs to be able to find, understand and use resources to make well-informed decisions about their health.1
Healthcare organizations have a responsibility to help make sure every patient has equitable access to the information and people needed to improve their health literacy and, ultimately, their quality of life.
Here are 5 ways your team can help make that happen.
1. Make patient education easy to understand

Whether through using PEMAT2 or consulting with a partner, take a good look at the materials you have to educate patients about their condition, medications and follow-up care needs.
For maximum comprehension of patient education, consider:
- Writing materials at a 6th grade or lower reading level3
- Including pictures & illustrations to help patients visualize key points
- Offering education in multiple languages, especially those most prevalent in your community & patient population
- Providing education in multiple formats (e.g., printed pamphlets, videos with closed captioning, voice commands, online & patient portal resources, dedicated phone lines)
- Prompting patients to review their education & automating alerts for nurse follow-up
These best practices not only help accommodate different learning styles, but also create more accessible avenues for patients to receive education.
2. Screen patients to assess health literacy
To get a baseline understanding of a patient’s analytical and conceptual skills—the same skills needed to make well-informed healthcare decisions—nurses can use screenings like the NVS tool.4
It’s also important to know a person’s social determinants of health and other risk factors that will likely affect their post-discharge outcomes.
Consider incorporating these patient screenings onto an interactive system to give nurses a consistent, efficient, and automated process for gathering patient data.
See why we recommend digital assessments
Once your nurses have an objective understanding of a patient’s health literacy and specific needs, they can more effectively plan their communications and follow-up strategies.

3. Communicate in a way that resonates
Being a good communicator5 with patients takes skill and, often, training. Here are some basics to keep in mind:
- Don’t let patients think you’re rushed or bothered. They want to feel heard, and your presence can help calm them. Watch your body language, maintain eye contact, nod while listening, sit down (if feasible), and ask questions that build rapport and trust.
- Talk casually with non-medical terms. Explain things like you would to a close friend, using common words (e.g., heart vs. cardiology, walk vs. ambulate, joints vs. orthopedics).
- Use teach-back methods6 to make sure patients understand what you’re saying throughout their stay.
- Know how to access real-time interpreters if patients are deaf, speak another language or have other special needs for communication.
4. Empower patients to take an active role
Even when clinicians aren’t in the room, you can keep patients engaged by empowering them with the information they want most while in your care.
For example, SONIFI Health partners with hundreds of healthcare organizations around the country to customize interactive in-room technology to fit their immediate needs and long-term goals.
Some of the platform features commonly used to help improve health literacy and outcomes include:
- Personalized interfaces that help orient patients & create simple paths for navigating to what they need
- Welcome videos & custom channels that teach patients how to use the in-room technology, ask for help, find education, access resources & learn about on-site services
- Condition-specific patient education that’s available on demand, automatically assigned & charted back into their EHR
- Detailed information about their care team & care plan so they understand who’s taking care of them, why they’re in the room, what their schedule for the day is & why certain procedures or consultations are happening
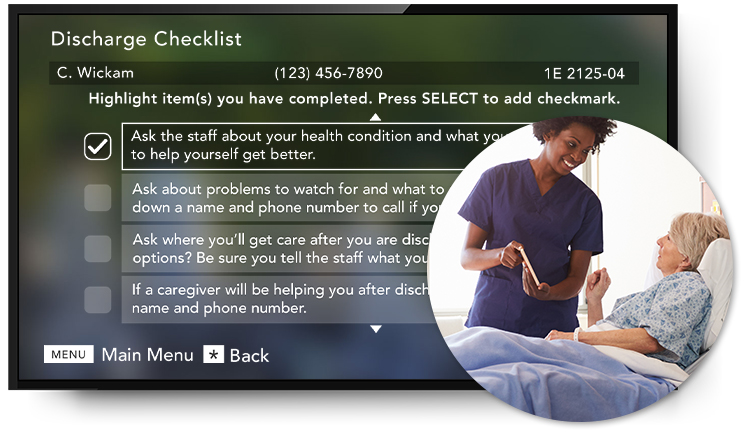
- Discharge checklists & dedicated discharge channels that give patients a clear understanding of the goals they need to meet before going home, as well as ideas for questions they may want to ask their providers
- Feedback & request features that provide an easy, immediate way for patients to let you know what they need or don’t understand yet—while also better preparing your team for effective bedside interactions
- Meds-to-beds prompts to prepare patients for success after discharge, improve medication compliance & reduce readmissions
5. Find the right partner for your journey to improve patients’ health literacy
Consider the value of having experts to consult with on best practices and new insights about how your team can help improve patients’ health literacy and overall experience.
SONIFI Health customers have access to professionals dedicated to nursing and education, analytics and outcomes, and ongoing success of your technology and goals.
Together with leading hospitals and healthcare organizations, SONIFI Health is helping evolve how effective and impactful patient engagement can be.
Stay connected
Get exclusive insights delivered to your inbox from our experts.
 By Lisa Branson, Nursing Executive
By Lisa Branson, Nursing Executive 